Descriptive Analysis of Anticoagulation Therapy Following Lung Transplantation
ABSTRACT
Background: Improved understanding of the clinical course of anticoagulated patients post-lung transplant may improve the prevention and management of thromboembolism and bleeding in this patient population.
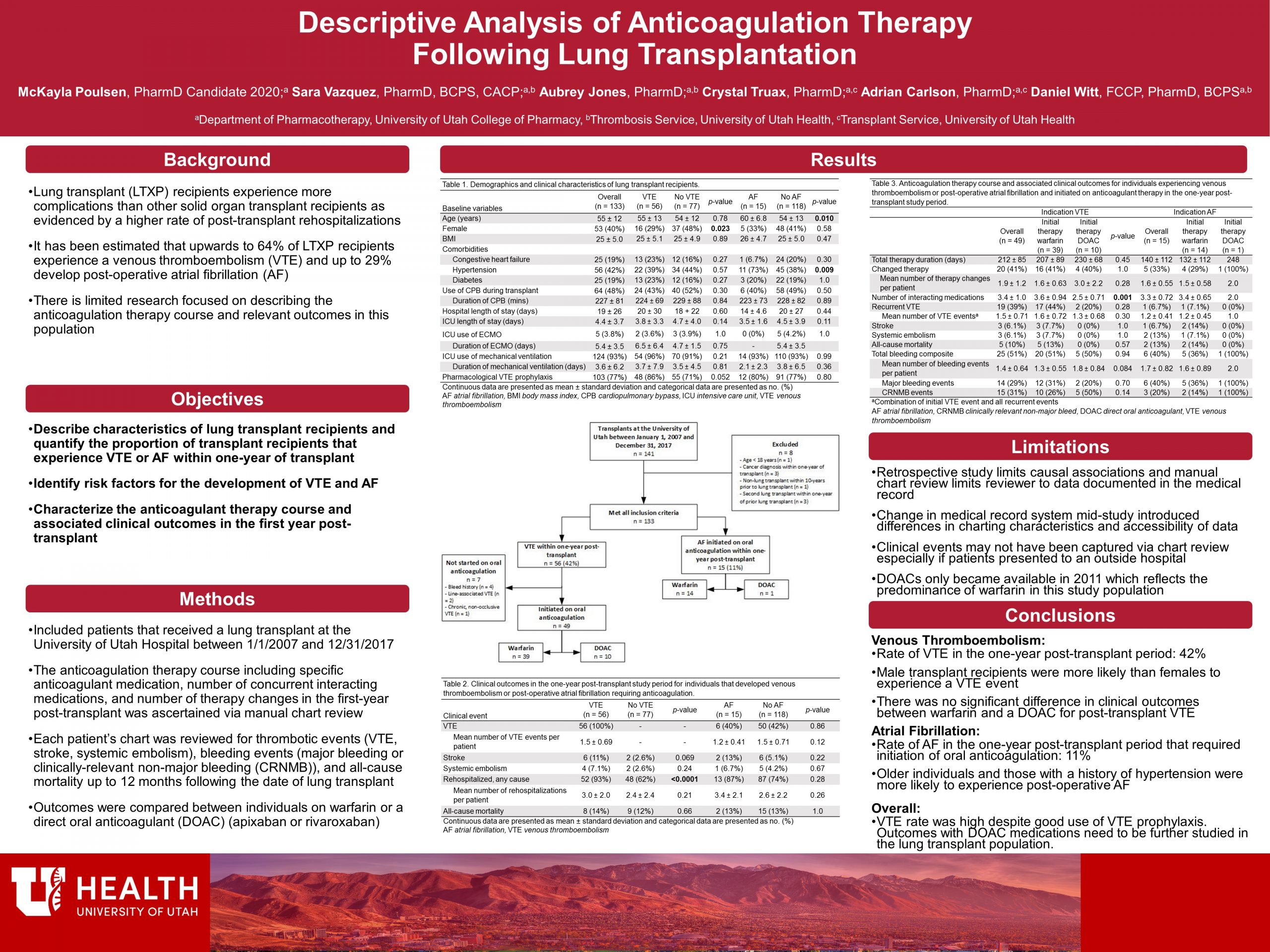
Methods: This single-center, retrospective descriptive study analyzed patients who received a lung transplant at the University of Utah Hospital between 01/01/2007 and 12/31/2017. The study population was assessed for basic demographic characteristics, risk factors for and development of venous thromboembolism (VTE) or atrial fibrillation (AF), and anticoagulant therapy course. Clinical outcomes of interest included recurrent VTE, stroke, systemic embolism, all-cause mortality, bleeding, and rehospitalization.
Results: During the study period, 133 patients received lung transplantation and were eligible for inclusion. Of those, 42% experienced a VTE in the first year post-transplant. Male sex was a risk factor for the development of post-transplant VTE (p=0.023). Of those experiencing VTE, 49 were initiated on anticoagulation, with 39 (80%) on warfarin and 10 (20%) on a DOAC. Rehospitalization (p< 0.0001) and any bleeding (p=0.001) were more common in patients that experienced a VTE as compared to those who did not.
Fifteen (11%) patients developed AF and began anticoagulation during the first post-transplant year. History of hypertension (p=0.009) and older age (p=0.010) were risk factors for the development of AF. All patients but one were initiated on warfarin, the other on a DOAC, and were more likely to develop major bleeding as compared to those without AF (p=0.019). There were no statistically significant differences in clinical outcomes between those started on warfarin versus a DOAC in the VTE or AF subgroups.
Conclusions: VTE and bleeding are both common occurrences in the lung transplant population. Additional studies are needed to determine the best anticoagulation therapy course to minimize these outcomes.
Published in College of Pharmacy, Virtual Poster Session Spring 2020
It amazed me to find that of all transplants, lung transplants have the most complications. Thank you for your research.
McKayla, Very nicely done! This looks quite comprehensive, and good to know that there does not seem to be a big difference in outcomes depending on nature of anti-coagulation used. Also good to see that VTE is a relatively rare event for people post-lung transplant.
Dr. Keefe,
Thank you for expressing interest in my research. It is difficult to relay a large amount of information on a poster so I couldn’t go as in depth about the VTE rate. One important thing about the previous study that identified a VTE rate of 64% for lung transplant recipients was that the study was prospectively looking for VTE and tested all transplant recipients, including asymptomatic patients. That is the only study with such a high rate – other studies were closer to 30%; so we were quite shocked to see a 42% rate of VTE!
Poster looks great McKayla! How often were bleeding events related to bronchoscopies?
Dr. Witt,
Overall about 10% of recipients had a bleeding event that was associated with a bronchoscopy. With 33% of all patients experiencing at least one bleed, the bronchoscopy events were certainly a fair proportion. Interestingly though is that there were no statistically significant differences in the rate of bleeding for bronchoscopy-associated bleeds across VTE positive vs. VTE negative patients – likely related to the fact that practitioners will interrupt anticoagulation therapy peri-procedurally. However, the non-bronchoscopy bleeds did reach statistical significance as well as overall bleeding (bronchoscopy and non-bronchoscopy combined).
Great analysis Mckayla. It appeared there were a number of recurrent VTE events. I am curious if you found a difference in the types of AC used and recurrence rates as well as timing of recurrence to the initial VTE event. I apologize if this was on the poster, I was not able to magnify to see some of your data in the charts.
Hey Kimmy,
Thanks for checking out my research. I have not analyzed time to recurrent VTE events; although, that may be something we might want to consider for the final manuscript. I did analyze differences in VTE recurrence between warfarin (44%) and DOACs (20%) but the difference was not statistically significant (p=0.28). The only statistically significant difference between warfarin and DOACs that we identified was that those individuals initiated on warfarin were generally on more concurrent interacting medications – which makes sense as starting an interacting medication was the most common reason found for switching from a DOAC to warfarin during our study.
Awesome job on your project, McKayla! Getting a better picture of how different risk factors could influence the chances of getting a VTE in this patient population is very intriguing.
Hi McKayla,
Great poster and research presentation. Sure excited you’ll be finishing up soon. Congratulations!
Great poster! It looks like this project gave you some good insight into the issues that lung transplant patients have with VTE risks. It looks like you put in a lot of hard work. Good job!
McKayla – What an awesome comprehensive job you have done. Like others – I was unaware of the high rate of VTE in this population. Nicely done.
Mckayla, wow! this is alot of data. i like the way you formatted the poster.