Provider Perspectives on Patients with a History of Atrial Fibrillation Not on Anticoagulation Therapy
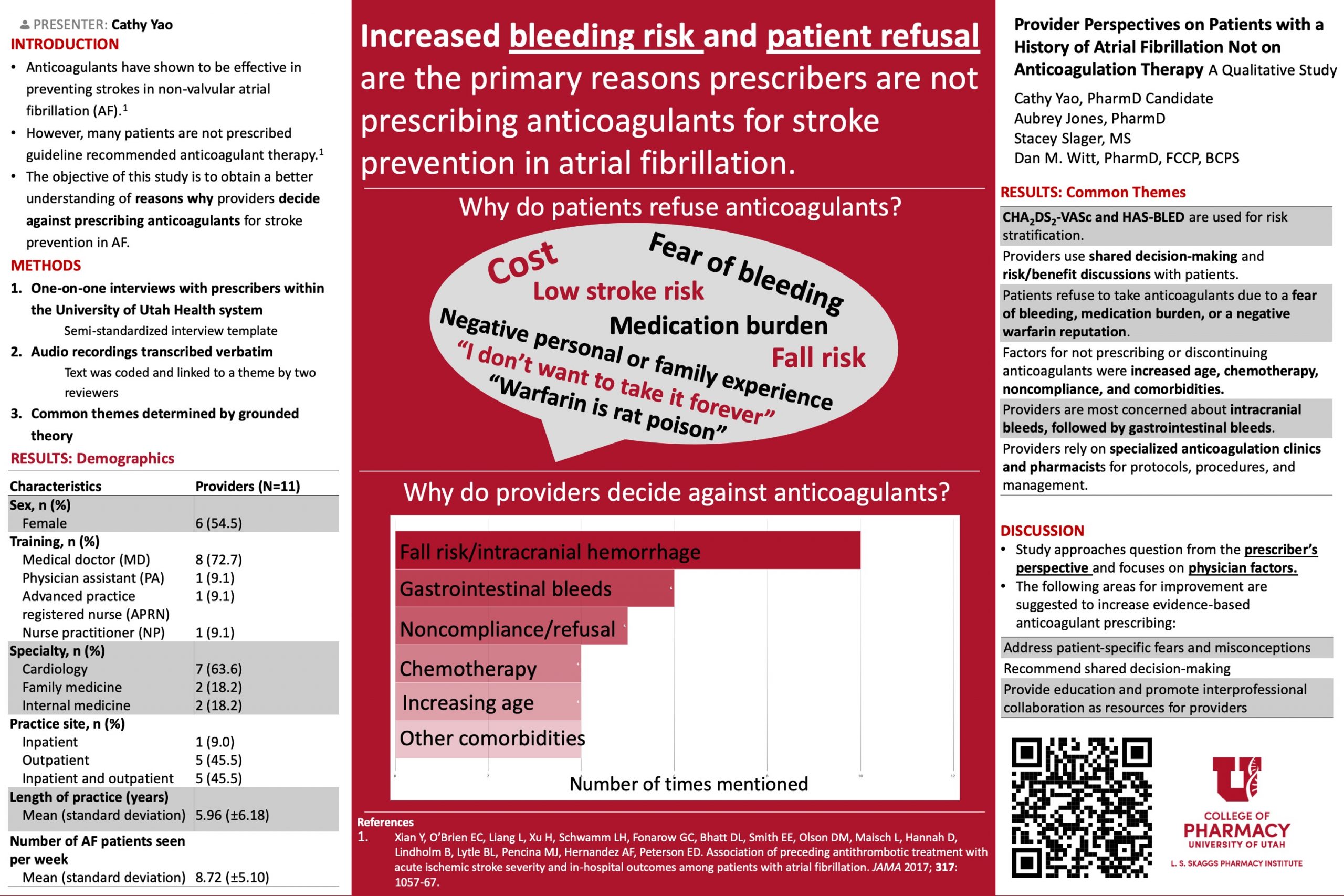
Background: Extensive data demonstrate the efficacy of anticoagulants in preventing strokes in patients with non-valvular atrial fibrillation (AF). However, many patients are not prescribed guideline recommended anticoagulant therapy.
Objectives: To identify themes underlying anticoagulant underutilization in patients with AF and compare and contrast prescribing preferences between cardiologists and general practitioners.
Methods: Providers practicing within the University of Utah Health system provided informed consent to be interviewed. A semi-structured interview template was used to guide the 15-minute interviews focusing on provider demographics and anticoagulant prescribing practices for patients with AF. Interviews were transcribed verbatim. Two reviewers independently read the transcripts and labeled passages of text corresponding with key concepts and themes. The number of interviews conducted was determined by saturation, or when major themes were established and no new themes emerged from further interviews.
Results: From the eleven practitioners interviewed, seven practiced in cardiology and four in general practice. The most prominent reasons cited for not prescribing anticoagulation for stroke prevention in AF patients were intracranial bleeds, followed by gastrointestinal bleeds. Other common factors for not prescribing or discontinuing anticoagulants were increased age, thrombocytopenia or chemotherapy, noncompliance, and comorbidities. Patient refusal of anticoagulants was due to a fear of bleeding, medication burden, or a negative reputation with warfarin. Providers had a similar prescribing strategy, including using CHA2DS2-VASc, having a shared decision-making discussion with the patient, and utilizing specialized anticoagulation clinics and pharmacists as resources.
Conclusion: Identifying major reasons directly from providers can be utilized to develop patient education addressing common fears and misconceptions, promote shared decision-making, and provide provider education and resources to achieve appropriate anticoagulant prescribing.
Published in College of Pharmacy, Virtual Poster Session Spring 2020
Hi Cathy,
Great job! Did you ask about the practitioner’s cut line on the use of the CHA2DS2-VASc score to determine the need for anticoagulation?
Thanks
Mark
Dr. Munger,
Thank you! We did not explicitly ask what CHA2DS2-VASc score the provider uses to determine the need for anticoagulation, although it would have been helpful as there is some debate. One provider mentioned that having a score of one is a gray area but they will still have a risk/benefit conversation with the patient. A couple of providers said that a score of 2-3 has a lower risk of stroke so if the patient has reservations about anticoagulants or concerning comorbidities, they will be less inclined to start an anticoagulant. Whereas, the provider would strongly recommend anticoagulants with a score was 5-6.
Please let me know if you have any additional questions!
Cathy, nice work! I enjoyed reviewing your poster. Do you agree with providers reluctance to prescribe anticoagulation due to fall risk? Why or why not?
Dr. Witt,
Thank you for all your help throughout this project! Many providers agreed that falls leading to intracranial hemorrhages are rare with anticoagulants; however, they are often detrimental or fatal to the patient when it does happen. Because of that, I would agree with the providers that it can be a valid reason to withhold anticoagulants in certain patients with a high fall risk. I thought it was interesting that some providers considered patients with diabetic neuropathy or a seizure disorder as having a high fall risk. I learned that these are additional factors to consider beyond frail, elderly patients being at risk.
Please let me know if you have any additional questions!
Nicely done, Cathy. It seems that your provider population was relatively new in terms of years of practice. Do you think the results would be different if you had responses from providers who had been practicing for longer?
Dr. Keefe,
Thank you! We did have some providers who were residents so I could see that affecting the results. I would suspect those who are new to practice may be more hesitant starting anticoagulants for patients with a higher bleeding risk. Additionally, they likely have not been able to follow a patient long-term and seen a patient have a stroke as a result of not being on anticoagulants or had a bleed from being on anticoagulants. However, many providers did mention that they try not to let previous experiences affect their prescribing habits and the decisions should be made for each specific patient. The smaller sample size is a limitation of this study and I would be interested in expanding so we could have input from a wider range in terms of years of practice.
Please let me know if you have any additional questions!
Cathy – Nice and important work!!! I wonder if you can compare what you found with other literature on the provider perspective. Do we find anything different from existing literature?
Dr. Chaiyakunparuk,
Thank you! We tried to structure our interview questions to address some of the provider-related factors that may affect anticoagulant prescribing habits based on current literature. For example, an article stated that some providers do not utilize the CHA2DS2-VASc score to assess risk, but all our participants said that they use it for all of their patients. Existing literature also discusses how some providers overestimate the risk of bleeding with anticoagulants – we specifically asked how frequent adverse events are with anticoagulants and whether this affects their prescribing habits. Many did agree that bleeding, specifically intracranial hemorrhages, is rare, but they do not let these events affect their prescribing habits. I believe we provided relevant supporting evidence for the existing literature.
Please let me know if you have any additional questions!
Cathy, this is a thoughtful methodology and study. Your data re-affirm that providers do have best interests of patient in mind. Would be interesting to learn their perspectives about shared-decision making, and clinical risk management.
Jim,
Thank you! I agree – a majority of the existing literature on this topic was chart reviews where it was reported that patients with high CHA2DS2-VASc scores were not on appropriate therapy. However, I think obtaining perspective directly from providers shows how they are working with the patient for the best decision based on multiple factors. For future studies, I suggested using a validated shared-decision making tool because it would be interesting to have quantitative results on this topic.
Please let me know if you have any additional questions!
Nice job Cathy. This is an important issue that may apply to other disease states – such as patients’ reluctance to use insulin or other medications that are viewed as “dangerous.”