Medication Compliance of Refugee and Spanish speaking Populations in Salt Lake County: An Initial Assessment
Abstract
Purpose: Refugee and Spanish-speaking populations are at high risk for medication noncompliance due to language and other barriers. Medication compliance is an action pharmacists can assess and use to encourage these populations to follow their prescribed treatment regimens and help modify behaviors. As the United States becomes more diverse, continued poor medication compliance among this high-risk population could result in serious public health and economic consequences. The purpose of this study is to collect and assess the medication compliance and potential barriers that may lead to medication noncompliance in refugee and Spanish-populations in Salt Lake County. The results will be used to identify where changes within a clinic can be made to better provide for these underserved populations.
Methods: This descriptive study was implemented using a survey to assess medication compliance of patients, in which English is not their first language. who fill at least one medication refill for a chronic condition. The study survey was performed at a single site clinic within the University of Utah Health system in Salt Lake City. Medication compliance was measured using the Brief Medication Compliance Assessment. Barriers to medication compliance were measured using the Adherence Start with Knowledge – 12 (Ask-12). Data collected was recorded in a secured excel spreadsheet.
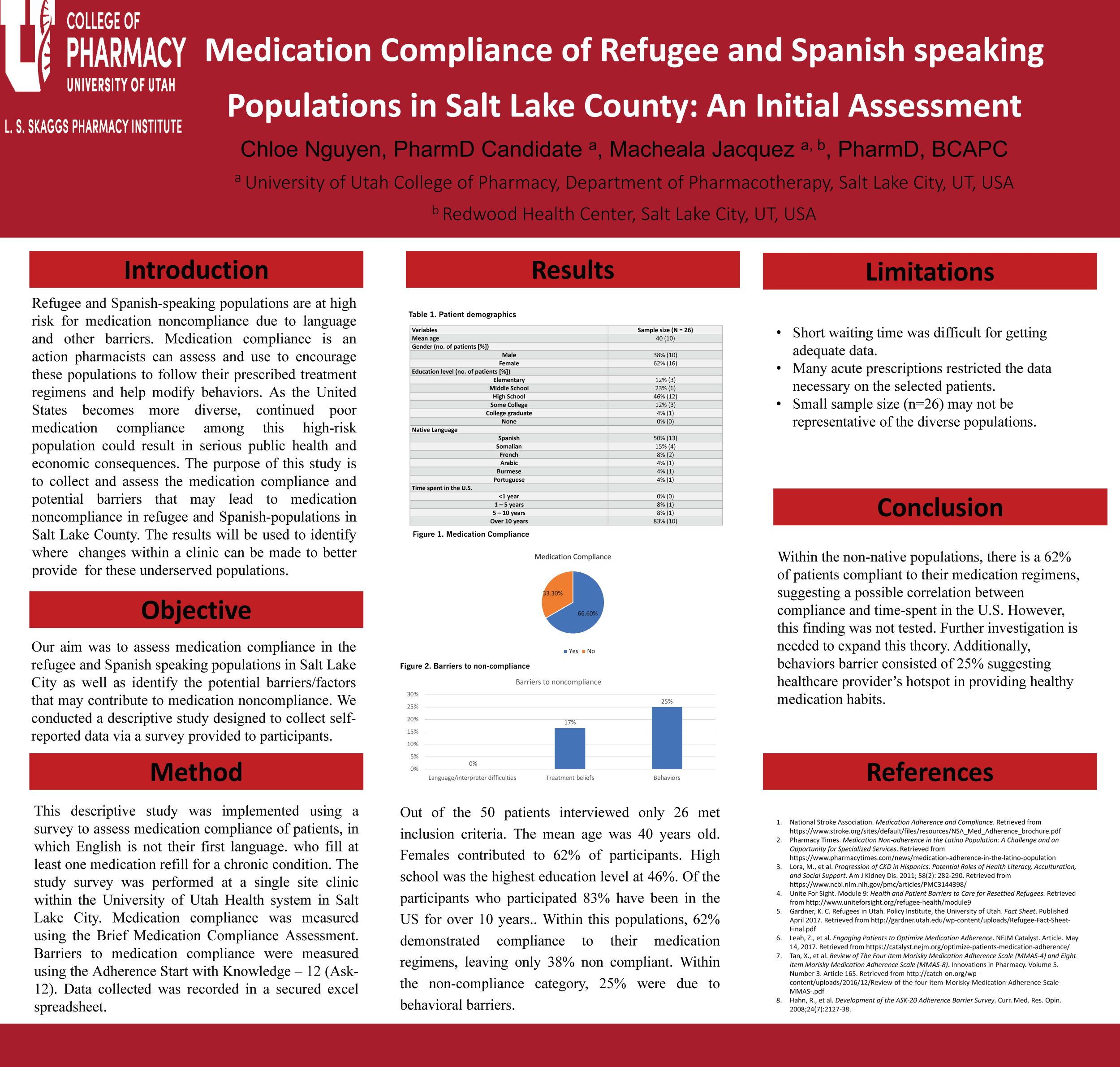
Results: Out of the 50 patients interviewed only 26 met inclusion criteria. The mean age was 40 years old. Females contributed to 62% of participants. High school was the highest education level at 46%. Of the participants who participated 83% have been in the US for over 10 years.. Within this populations, 62% demonstrated compliance to their medication regimens, leaving only 38% non compliant. Within the non-compliance category, 25% were due to behavioral barriers.
Conclusion: Within the non-native populations, there is a 62% of patients compliant to their medication regimens, suggesting a possible correlation between compliance and time-spent in the U.S. However, this finding was not tested. Further investigation is needed to expand this theory. Additionally, behaviors barrier consisted of 25% suggesting healthcare provider’s hotspot in providing healthy medication habits.
Published in College of Pharmacy, Virtual Poster Session Spring 2020
Chloe, very well done. It is so nice to see the study once completed! While your sample size is small, I found the results encouraging that the majority of patients you were able to interview were adherent to their medications. Do you have an idea of what the behavioral limitations are for those who were not adherent? Also, I’m curious, were men more likely to be non-adherent, or was the distribution similar to the overall distribution of males and females in the study?
Well done Chloe! I had the same question- what are some examples of the behavioral barriers that tended to be present? Thanks for sharing!
Hi Brynne,
Thank you for your question. Here is the list of questions in the Behavior category:
– Have you ever taken a medicine more or less often than prescribe?
– Have you ever skipped or stopped taking a medicine because you didn’t think it was working?
– Have you ever skipped or stopped taking a medicine because it made you fee bad?
– Have you ever skipped, stopped, not refilled, or taken less medicine because of the cost?
– Have you not had medicine with you when it was time to take it?
These are Yes/No questions with “Yes” being 2 points, and “No” is 1 point. The higher the point the more barrier perceived.
Hi Dr. Keefe,
Thank you for your feedback!
For the first question, I used the ASK-12 section to determine the barriers. This subgroup included 12 questions with “Yes”, and “No” responses. Answer “Yes” received 2 points whereas “No” is 1 point. The higher the point the more barrier perceived. These 12 questions then divided into 3 categories: Language/Interpreter difficulties, Treatment beliefs, and Behavior. Within the Behavior category, we asked patients to see if they have ever stopped taking medications due to side effects, cost, or forgetfulness. The majority of our patients said that side effects were the main reason for their non-compliant.
For the second question, I don’t have the answer to it. This is a very good question. As our study showed that our sample size is very small with the majority of participants being female, I don’t think our findings would be significant to draw out the compliant rate difference between genders. We just measured the complaint rate as a whole.
Chloe, interesting work. I wonder how compliance is measured using the Brief Medication Compliance Assessment. Is that like a questionnaire? Is it self-reported? I’d like to hear your thoughts on the limitation of this tool. In addition, I wonder if the tool has been well validated in Spanish language. Do you have any information on reliability and validity test findings of this tool?
Hi Dr. Chaiyakunparuk,
Thank you for your questions and feedback!
We developed this self-report survey to assess medication compliance in these selected populations. The Brief Medication Compliance Assessment consists of 4 multiple-choice questions. The first 3 questions were used to determine if the patients were eligible to participate in the compliance assessment. For example, there were two responses to the question “Are you currently taking any medication?”. Reply “Yes” is indicated that the prospective participants are applicable in participating in this study. Answer “No” is eliminated from this assessment. The question: “How often do you take your medication as described?” is used to assess medication compliance. Responses for this item were ranging from “Always”, “Often”, “Sometimes”, “Occasionally”, and “Never”. The cutoff point for non-compliant is when the participants answered either “Sometimes”, “Occasionally”, and “Never”. Additionally, I have not found any literature in regard to the tool for assessing medication compliance in non-English speaking populations. We developed this tool using our considerations upon these populations.
There are several limitations to this study. First being time. Surveying patients while they wait for prescriptions and getting adequate data in a short amount of time was difficult. Most patients were not interested due to their short wait time at the pharmacy. Numerous surveys were interrupted by the pager, a device signaling their wait time is up for prescription pickup, and ended the survey early. Only a few patients returned to finish answering questions. Secondly, many of the pharmacy patients were just in the clinic for acute prescriptions. This issue restricted the investigators to collect more data necessary for the selected patients. Thirdly, many patients who declined to participate in the study despite the help of an interpreter via an IPad. Most of the patients who agreed to the survey already had a fairly good grasp of the English language. This bias could be a reason the final results did not match the hypothesized results because those that understand English well have previously been shown to comply with their medication regimens. Lastly, the survey done while patients picking up medications to determine whether or not the patient is compliant is self-limiting. Only those who are currently taking medication will be assessed. This limits our data pool.
Nice job, Chloe. I was surprised to see that no patients noted language as a compliance barrier. What were some findings that surprised you?
Hi Dr. Witt,
Thank you for your question. I agree that this finding is contradictory to what we have predicted prior to the study. We thought that medication compliance will be low within refugee and Spanish speaking populations. However, the results showed that 62% of the Redwood Clinic patients compliant to their regimens. This surprised me quite a lot. Nevertheless, these results make sense when we put some factors into consideration. First of all, these patients were being interviewed with the help of the interpreter (either in person or via an iPad). Secondly, the majority of participants that agreed to our study were those that have been living in the U.S for more than 10 years. This could somehow explain the fact that these patients are more likely familiar with Western healthcare systems and are familiar with expectations of taking their medications as directed by the providers. Although, we encountered many limitations that could provide some bias to the study. We are looking for further investigation into these populations in the near future.
Great job Chloe. I am with Dr. Witt and surprised that none of the patients put language as a barrier to their adherence. In my experience, I have found that language can be a big barrier in the pharmacy. I wonder if they rely on their medical provider for their prescription information and this is why they didn’t put language as a barrier.
How does this 62% compliance compare to the compliance rates other demographic groups, such as English-speaking, and so on? This research topic is quite interesting and significant.
Interesting poster! The topic is definitely an important one for pharmacists who work with diverse populations. Given that you have done much data collection, what do pharmacists need to do to find fewer barriers in the future? I liked the presentation of your poster. Thank you.
Hi Nguyen,
Nice poster and important study. Salt Lake has such a diverse population with many languages.
Thanks for the presentation. Sure excited that you’ll be finishing soon! Congratulations!
medication regimens
Chloe, nice job. Your work brings renewed awareness to the idea that effective communication is the key to …. everything.