Evaluation of Bleeding Events Associated with a Risk Stratification Protocol in Post-op Arthroplasty Patients
SUMMARY
Background: The University of Utah developed a risk stratification protocol to determine which medication, warfarin or aspirin, is prescribed to patients undergoing joint arthroplasty procedures based on risk for venous thromboembolism (VTE) and bleeding.
Objective: To validate the belief that a risk stratification protocol to determine postoperative VTE prophylaxis after primary total hip arthroplasty (THA) or total knee arthroplasty (TKA) lowers bleeding events compared to prescribing anticoagulation for all patients regardless of VTE risk.
Patients/Methods: Retrospective cohort study using data obtained from electronic medical record review of arthroplasty procedures at the University of Utah Hospital. Bleeding rates during the 90-day post-op period were compared between a cohort of TKA/THA patients prescribed warfarin in 2013 to patients prescribed warfarin or aspirin based upon risk stratification in 2017.
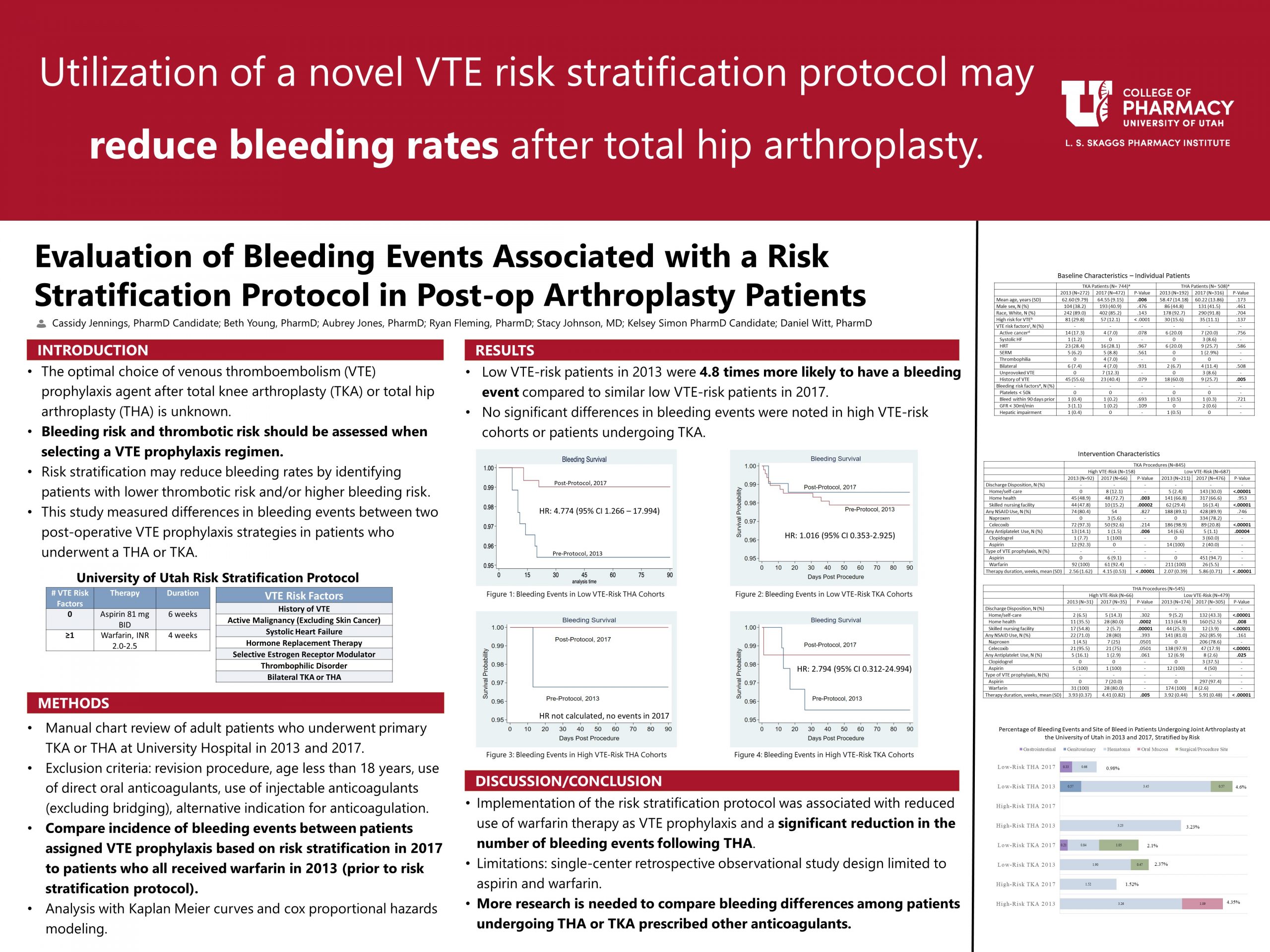
Results: 1,390 procedures were identified. The unadjusted hazards ratio for major bleeding after THA surgery in low-risk patients in 2013 vs 2017 was 4.774 (p=.021; CI 1.266 – 17.994), suggesting a lower rate of bleeding with the use of the risk stratification protocol. Bleeding rates were similar among TKA and high-risk groups and results were not statistically significant.
Conclusions: Utilizing a risk stratification protocol to determine VTE prophylaxis resulted in lower major and clinically relevant non-major bleeding events after THA surgeries. Further study is needed to clarify bleeding risk after TKA procedures.
Published in College of Pharmacy, Virtual Poster Session Spring 2020
Nice work, Cassidy! When you consider your results in conjunction with Kelsey’s do you think other healthcare systems should institute risk stratification programs for their joint replacement populations? Why or why not?
Thank you for the interesting study. I was curious what was defined as high vs low risk? Was it just based on the # of risk factors (>=1 was high risk)? Is this a validated tool that is used to risk stratify? I saw there was more bleeding associated with the Low VTE risk patients and was curious if at the time of bleeding event was it associated with low PLTs or supratherapeutic INR or other hematologic levels? I also wondered what the occurrence of VTE was in the low vs high risk group? I saw in the baseline group, there were quite a few (~50%) with provoked VTE hx. Thank you!
Dan:
I think that the combination of my results – reduced risk of bleeding events – and Kelsey’s results – similar VTE events – suggest that establishing a risk stratification protocol can be successful in a healthcare system in minimizing bleeding and VTE risks. I think that other institutions should consider adopting a risk stratification protocol as it reduces the use of anticoagulants, reduces some burden on the healthcare system by decreasing the need for INR monitoring, and remains effective. Furthermore, aspirin as an option for VTE prophylaxis in low-risk patients reduces drug interactions and is easily accessible for patients as it is both inexpensive and available over the counter. Something to consider before implementing a risk stratification protocol is how the risk assessment will take place, who will conduct the risk assessment, and how the institution will evaluate both adherence to and effectiveness of their protocol. I think realistically that more studies will need to be done, especially studies including risk stratification and other VTE prophylaxis options (DOACs specifically), before this is widely implemented.
Kimmy:
I have numbered my responses to your comments/questions to hopefully make it easier to read:
1. You are correct on the first point. High-risk patients were defined as having one or more risk factor for VTE listed in the table (Hx of VTE, active malignancy, systolic heart failure, hormone replacement therapy, SERM, known thrombophilic disorder, or bilateral TKA/THA).
2. This risk stratification protocol is not a validated tool; the purpose of this study was to gather data on the effectiveness of this tool to help validate its use in clinical practice.
3. Due to the way we gathered data and that the data from 2013 was pulled from an older charting system, we were not able to identify supratherapeutic INRs/PLT levels at the time of bleeding events. That would be an interesting area to dig deeper and do further study to clarify higher incidences of bleeding.
4. I did not evaluate the results of VTE occurrence – but I can direct you to the poster of my colleague that worked on this project with me and analyzed the VTE event results. The author is Kelsey Simon and the poster is entitled “Evaluation of VTE Risks Associated with a Risk Stratification Protocol for Venous Thromboembolism Prophylaxis in Post-op Arthroplasty Patients”
Thanks for your questions! I appreciate your time and thoughtfulness regarding my project.
Cassidy, very interesting study. Do you think the difference between the TKA and the THA reflects differences in the nature of the surgical procedures and, therefore, the propensity for hematoma/surgical site bleeds? Also, excellent, scholarly responses to the questions already raised!
Kristen:
Thanks for your question! I think the differences in bleeding seen between the TKA and THA cohorts are likely due to the low incidence of bleeding overall. However, it is possible that it is also influenced by the differences in the propensity for bleeding between surgeries. TKA procedures are associated with longer recovery times and the joint is very close to the surface, whereas the hip joint is covered by more layers of muscle. This would be an interesting area for further research.
Cassidy – This is an interesting work!!. Wonder if you know of any literature comparing this risk stratification tool and those pre-protocol. Just wonder if this has tool has been recommended in any Clinical practice guideline yet. IF not, will your work be a good evidence to support changes in CPG in future? What do you think?
Nathorn:
There are a few studies that include risk stratification tools or suggest the use of risk stratification, but this tool is not yet recommended in clinical practice guidelines. In fact, the two major guidelines (American College of Chest Physicians [ACCP] and the American Academy of Orthopedic Surgeons [AAOS]) are both due for updates, being last published in 2012 and 2011 respectively. I think that my study could be considered as evidence to support changes to the guidelines, but more research is needed to support my findings before any solid changes can be made.