Comparing the Efficacy of Polyethylene Glycol 3350 to Docusate Sodium in a Neuro Critical Care Unit Bowel Regimen
Background/Objective:
Poor bowel function is a risk for patients in the Neuro Critical Care Unit (NCC). Many medications are used to manage poor bowel function. Retrospectively, we compared a scheduled once-daily polyethylene glycol 3350 (PEG) to scheduled twice daily docusate sodium (DS) for improvement in patient bowel function as part of an NCC bowel protocol. The lack of evidence to support the efficacy of docusate in primary literature prompted a change in the bowel regimen in December of 2016 to improve patient bowel function and decrease complications related to constipation.
Methods:
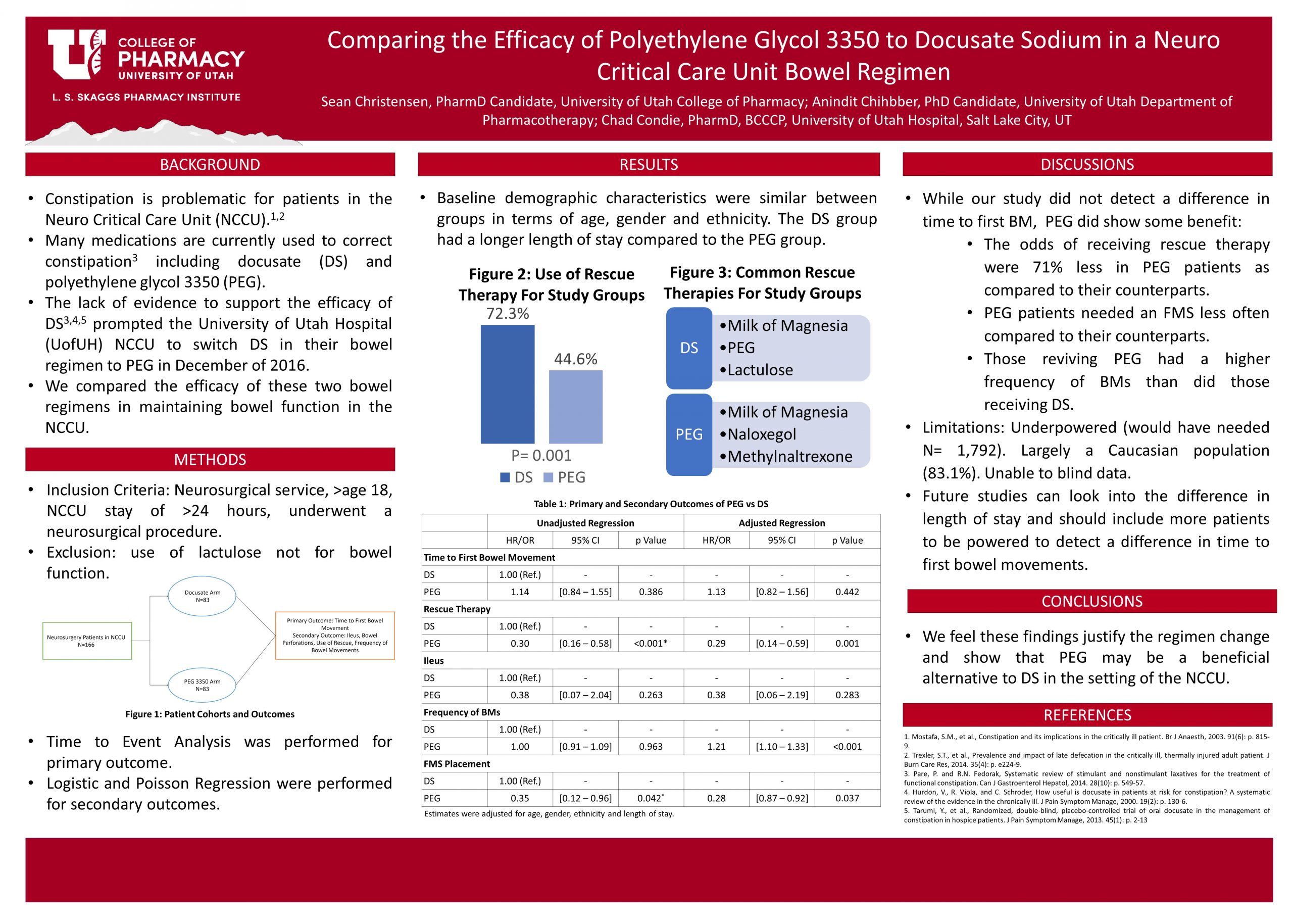
We included inpatient neurosurgical patients age 18 or higher who underwent a surgical procedure and spent at least 24 hours in the NCC. A total of 166 patients were included, 83 using docusate before the regimen change, and 83 using PEG after the change. Data were collected from the electronic medical record (EMR) and included baseline demographics/characteristics, time-to-first bowel movement (primary outcome), use of rescue therapies, number of bowel movements, ileus, and bowel perforation. Time-to-event analysis was performed for the primary outcome while Logistic and Poisson Regression were performed for secondary outcomes.
Results:
Baseline characteristics were almost similar between groups; the length of stay was longer in the DS group. There was no statistical or clinical significance in the primary outcome. There was a statistically significant decrease in the use of rescue therapy in the PEG group with an OR of 0.29, 95% CI [0.14-0.59], and a p-value of 0.001. Placement of FMS was also lower in the PEG group with an OR of 0.28, 95% CI [0.87-0.92], and a p-value of 0.037.
Conclusion:
PEG did not decrease time to first bowel movement relative to DS but showed a statistically significant reduction in the use of rescue therapy and fecal management system placement, which we feel justifies the change in bowel regimen. These findings can help guide clinicians in the choice of bowel regimen in the NCC.
Published in College of Pharmacy, Virtual Poster Session Spring 2020
Interesting study and the important results you determined.
Thank you!
Great poster, Sean, and very interesting. Are the common rescue therapies for each group listed in order of how frequently they were used? (Figure 3) Do you have the breakdown of percentage use for each of these individual rescue therapies?
Thanks Spencer, yes they are listed in order of highest frequency used. The breakdown for the top three in each group are as follows. Of those who received rescue therapy in the DS group 76% got milk of Magnesia, 56.7% got PEG, and 40% received lactulose. Of those who received rescue therapy in the PEG group, 81.1% got milk of magnesia, 73% got naloxegol, and 16.2% received methylnaltrexone. I can provide the whole list if you have further interest.
Thank you! And yeah, if you have that full list, I would like to see it! (Largely due to the similarities of our projects.)
Here is the list of rescue therapies and their utilization rates.
Rescue Therapies Used (first column DS second column PEG)
Milk of Magnesia 46 (76%); 30 (81.1%)
Lactulose 24 (40%); 0 (0%)
Magnesium Citrate 5 (8.3%); 5 (13.5%)
Naloxegol 4 (6.7%); 27 (73%)
Methylnaltrexone 20 (33.3%); 6 (16.2%)
Fleet Enema 2 (3.3%); 0 (0%)
SMOG Enema 4 (6.7%); 1 (2.7%)
PEG 34 (56.7%)
Sean, well done! Your poster is quite clear and easy to follow. It looks like the change made in 2016 was a good one and has led to better outcomes for the patients. I’m not familiar with the term “FMS”. What is that?
Thank you Dr. Keefe, and I am sorry for the confusion with the FMS. Somehow the full name got taken out of the abstract and the poster in the editing process. I will have to update that. FMS stands for Fecal Management System. They are a catheter based system used to keep the skin clean and dry to prevent skin breakdown when an individual has diarrhea (liquid or semi liquid consistency) and fecal incontinence.
Great job Sean! I don’t know if it is just me, but I think it is so fun seeing research from institutions that you work at! This is likely beyond the scope of this project, but was there any discussion regarding the use of concomitant therapies (narcotics, anticholinergics, etc.) that may have contributed to the heightened requirement of rescue therapies between the two groups? Further, I think an important aspect to consider in regards to choice in treatment would be volume restrictions set for the patient?
Thanks KC, and yes there was some discussion regarding the use of constipating (for lack of a better term) medications. All of these patients were post neurosurgical patients and were thus all on opioids and had that complicating factor. Hence the importance for finding a bowel regimen that is going to be appropriate for this population. We did not look at which specific agents and doses/duration were used for this project. As far as volume restrictions are concerned that is not something that we looked into. That could be an interesting factor to take into account for projects of this nature in the future. Thank you for your thoughtful questions.
What a great project! The poster is informative and easy to read. Very timely study.
Nice project. Did you by chance find differences in specific patient characteristics such as spinal cord injuries? I also wondered if the placement of an FMS means that PEG based bowel regimens may be too aggressive since the number of BM’s and consistency have to be quite significant for an FMS to be used? Use of FMS isn’t without its own level of complications. Also I noticed this analysis focused on medication use in the two protocols. Were there any differences in the use of “below the belt” bowel regimen use such as suppositories, enemas, or dig stim? Thank you.
Thank you for your questions, these are all great thoughts. To answer your first question: we did not adjust for the type of injury or type of procedure performed. The type of procedure performed was collected when available in the chart and can be used in a future analysis/study but was not something we had the means to assess for this project. It would be very interesting to see a project that took those factors into account, great thought! To your second point about the FMS placement, as you can see in the results, there was actually less FMS placement with the PEG group relative to the DS group. The odds of having an FMS placed were 0.28 times as likely with PEG compared to DS. So I would agree that more FMS placement would indicate that a given regimen may be too aggressive. Our thought was, it is a possibility that more FMS placement in the DS group could have been because they required rescue therapy more often. The rescue therapy needed to produce a bowel movement may have caused more diarrhea on the back end after the initial BM was produced. To your third question, the DS group did report more enema use although those numbers a merely descriptive, we did not perform any analysis to see if that increase was statistically significant (you can see the numbers referenced under my last response to a comment from Spencer Simister above). As you point out our focus was on the differences in the medications used in the two bowel protocols. The two bowel regimens in this study from did not include any information outside of medications so we did not collect information about whether dig stim was performed. This would also be an interesting point to include in a future study. Thank you!
That’s a very practical study— not only in neurosurgery, they always are sending you home from surgery with DS. I’ve had better results with PEG… congrats on your new findings.
Thank you Dr. Lim!
Sean, I enjoyed being in your review group for the last couple of semesters. You have put an immense amount of work into your project, and it shows – nice work! I was curious if you had any thoughts about adherence and if adherence played a role at all in the results of this study?
Thanks Sam, the question about adherence was something that we thought about but did not control for this this particular study. We worked under the assumption that since the medications were being administered by nursing staff that both arms of the study were adherent to their respective regimens. Spencer Simisters project (the sister project to this study) on the other hand did look at adherence to the Bowel regimen and the role that played in the Neuro Acute Care Unit. great thought!
Great job Sean! I thought you did a great job on your poster and study.
Thanks Robbie!
Interesting topic that has been ongoing for decades with Docusate!! Glad you tackled this topic for this specialized patient population! A few minor questions involve: What is FMS? What dosages of Docusate and PEG were utilized? Also, how were fluids assessed for this population since hydration is important for both agents. Is there also a cost savings regarding your findings? Your study, Sean, has made important discovery for this specialized unit. Nice work! Thank you.
Dr. Orlando, Thank you for your thoughtful comments and questions.
About FMS: I am sorry for the confusion with the FMS. Somehow the full name got taken out of the abstract and the poster in the editing process. I will have to update that. FMS stands for Fecal Management System. They are a catheter based system used to keep the skin clean and dry to prevent skin breakdown when an individual has diarrhea (liquid or semi liquid consistency) and fecal incontinence.
The dosage of docusate being used was 100 mg twice daily scheduled for the DS arm and no one one received docusate in the PEG arm.
Fluids: we did not assess fluids in this particular study. We worked under the assumption that as patients in NCC they were managed either by IV fluids or PO if able. This is a good point to bring up though as you stated, adequate fluid intake is essential for these medications. Proper hydration should be a factor included for future projects in this area.
Cost: we did not directly assess cost as part of this project either. Although it can be hypothesized that a decrease in the use of rescue therapy as well as less use of FMS in the PEG arm will be cost saving in product (medication and FMS tubes). This is another potential area of future exploration that can be assessed in this population.
Great job on this project! It will make a difference clinically.
Thank you Dr. Tyler!
Sean, nice work. I know it was not part of the study design, but do you happen to know if there is a substantial difference in cost?
Thank you for the comment Dr. Ruble, and good question. I did not look into the cost although it would be a natural next step and something that may be looked at in the future. Hypothetically, since the PEG group had less rescue therapies used and had less FMS (fecal management system) placed, it is very possible that there could be a cost savings associated with PEG. That is something that we speculate as a possibility in the manuscript but would need to do more analysis to show. Thanks again, let me know if you have any further questions.
Sean, good work! I found your poster to be very informative and exciting after seeing that often DS is preferred as the first line bowel regimen throughout my rotations. Although these findings are in a specific population, your results spark my curiosity in other populations.