Christensen Sean
Comparing the Efficacy of Polyethylene Glycol 3350 to Docusate Sodium in a Neuro Critical Care Unit Bowel Regimen
April 29, 2020 in College of Pharmacy, Virtual Poster Session Spring 2020
Background/Objective:
Poor bowel function is a risk for patients in the Neuro Critical Care Unit (NCC). Many medications are used to manage poor bowel function. Retrospectively, we compared a scheduled once-daily polyethylene glycol 3350 (PEG) to scheduled twice daily docusate sodium (DS) for improvement in patient bowel function as part of an NCC bowel protocol. The lack of evidence to support the efficacy of docusate in primary literature prompted a change in the bowel regimen in December of 2016 to improve patient bowel function and decrease complications related to constipation.
Methods:
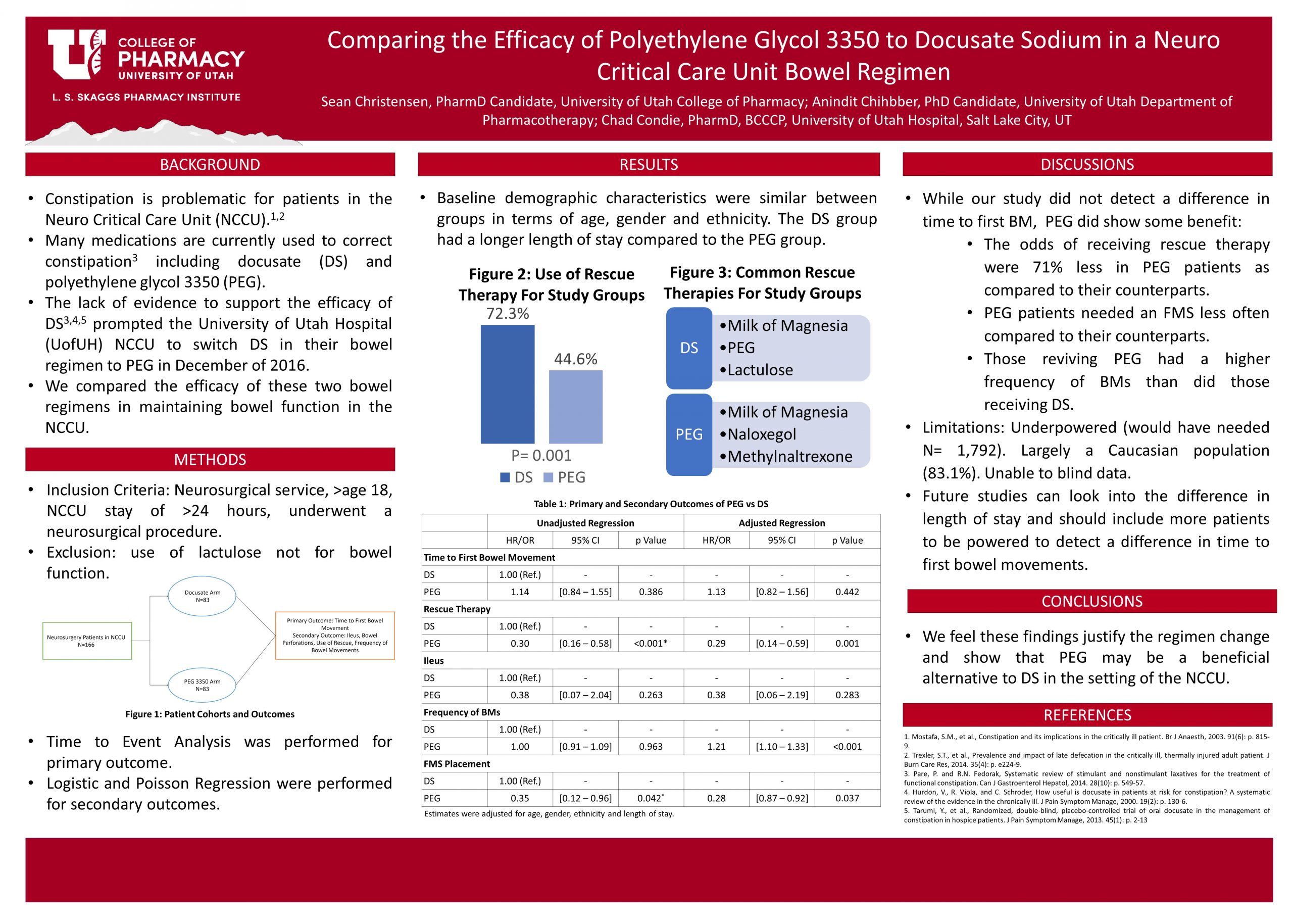
We included inpatient neurosurgical patients age 18 or higher who underwent a surgical procedure and spent at least 24 hours in the NCC. A total of 166 patients were included, 83 using docusate before the regimen change, and 83 using PEG after the change. Data were collected from the electronic medical record (EMR) and included baseline demographics/characteristics, time-to-first bowel movement (primary outcome), use of rescue therapies, number of bowel movements, ileus, and bowel perforation. Time-to-event analysis was performed for the primary outcome while Logistic and Poisson Regression were performed for secondary outcomes.
Results:
Baseline characteristics were almost similar between groups; the length of stay was longer in the DS group. There was no statistical or clinical significance in the primary outcome. There was a statistically significant decrease in the use of rescue therapy in the PEG group with an OR of 0.29, 95% CI [0.14-0.59], and a p-value of 0.001. Placement of FMS was also lower in the PEG group with an OR of 0.28, 95% CI [0.87-0.92], and a p-value of 0.037.
Conclusion:
PEG did not decrease time to first bowel movement relative to DS but showed a statistically significant reduction in the use of rescue therapy and fecal management system placement, which we feel justifies the change in bowel regimen. These findings can help guide clinicians in the choice of bowel regimen in the NCC.
