Abstract
Purpose
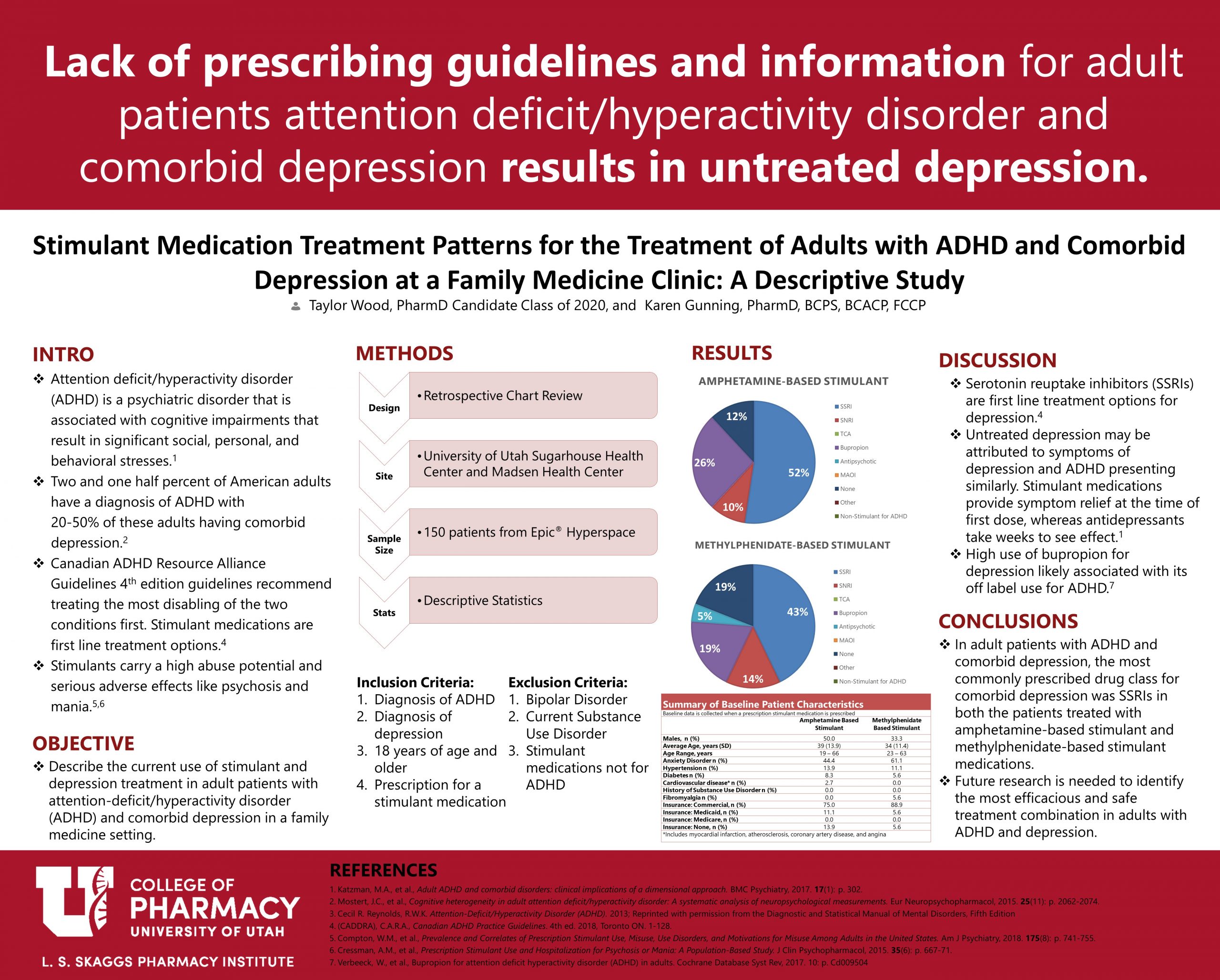
Attention-deficit/hyperactivity disorder (ADHD) is a psychiatric disorder that results in significant social, personal, and behavioral stresses. Adults with ADHD have a high prevalence of comorbid psychiatric comorbidities, with major depressive disorder (MDD) occurring in 20-50% of patients. Current guidelines recommend treating the more disabling of the two conditions first leading to many patients treated with stimulants alone. Stimulant medications are not without risks and do not treat, and may exacerbate concomitant mental health conditions. Therefore, the objective of this study is to understand the current use of stimulant and other medication therapies in adult patients with ADHD and comorbid depression in a family medicine setting, in order to improve care, safety, and reduce adverse effects.
Methods
This descriptive retrospective chart review sampled patients of a family medicine clinic. Patients included were 18 years or older, had a diagnosis of ADHD and depression, and were prescribed a stimulant medication. Medication treatment patterns were described by drug class.
Results
35 patients were treated with an amphetamine-based stimulant and 17 were treated with a methylphenidate-based stimulant. The most commonly prescribed treatment for depression was a selective serotonin reuptake inhibitors (SSRIs) with 9 patients having no depression treatment.
Conclusions
In adult patients with ADHD and comorbid depression, the most commonly prescribed drug class for depression was SSRIs in both the patients treated with amphetamine-based stimulant and methylphenidate-based stimulant medications. Future research is needed to identify if this is the most efficacious and safe treatment combination in adults with ADHD and depression.
Taylor, nicely presented. I was heartened to see that the majority (albeit not 100%) of people with co-morbid ADHD and depression are, in fact, receiving treatment for both conditions. I wonder if there is a difference in patients being treated with non-stimulant medications for ADHD?
Hi Dr. Keefe,
That was exactly one of my thoughts when I was collecting data! I think there are so many ideas for future studies in this patient population and the data would result in better QoL for these patients.
Great job Twood! I am curious to your thoughts on whether or not bupropion could be an appropriate first-line option for those individuals who may be suffering from depression, but would likely benefit from the off-label indication for ADHD? It does vary from our conventional practice, but maybe could help some patient populations without the addition of a stimulant? Certainly gets my wheels turning.
Hi KC,
That is a great question and something that I think needs to be investigated further. Currently, there is weak evidence for the use of bupropion in patients with ADHD without combination of a stimulant. To my knowledge, there are not any studies combining both stimulants and bupropion in these patients. My concern with this combination is that both medications act on Dopamine and Norepinephrine which may result in more adverse events. Because of this, I am hesitant to recommend this as first-line rather than an SSRI for treating depression until we have more data.
Great job! It would be interesting to be able to follow up to see how patients respond to different therapies.
Hi Dr. Lim,
I totally agree with this thought and I also shared the same thought when I was collecting data. I think this would be a great idea for future research at our clinics.
Fantastic poster Taylor! I’ve definitely been seeing these treatments (ADHD and depression) more frequently. I’d be interested to see more information of when these patients received a diagnosis of depression. Would it be before or after their ADHD diagnosis?
That is a great thought Ashley! Because these symptoms can mimic each other, I wouldn’t be surprised if the diagnosis of depression was missed for many years during ADHD treatment. This is an interesting topic for future research 🙂
Good poster, Taylor. I had a question about your inclusion criteria. Why did you only include patients who were currently taking a stimulant medication? Was there a reason that patients taking atomoxetine (Strattera) or FDA-indicated ADHD treatment were not included? Thanks!
Hi Brynne,
The focus of the study was geared towards stimulants only due to the risks of these medications and lack of research. I think it would be really interesting to look at non-stimulant medications as well! I would not be surprised if the findings would be similar in both populations. Great thought and definitely a topic for future research 🙂
Hi Taylor, awesome job on your poster! I am happy to see that no patients were on an MAOI while on a stimulant medication in your results. I also agree with KC that it will be interesting to see if bupropion would be a viable option for this patient population.
Taylor- great poster! It was interesting to see such as high level of comorbid anxiety in this patient population being treated with stimulants. It would be interesting to see how the additional diagnosis of anxiety might impact treatment decisions for ADHD.
Hi Taylor! What an informative poster! Since I do not work with this pt population directly, I was not aware of the therapeutic dilemma that you have thoughtfully investigated. What do you think is the next step the community-based and/or clinic pharmacist can be involved to assist with management of these pts? Very nice work. I liked your formatting selections for the poster. Thank you.
Taylor –
Nice job answering questions! So many future studies could be done – especially on a wider scale – thank you for delving into this this year!
dr g
Great project!
Taylor – what a fascinating topic. I love how you were able to identify a research question and map out the findings. Very nicely done! Congrats!!
Taylor, this is a great project. Utah is frequently criticized for “irrational” prescribing of neuropharmacology therapies. it is good to see studies, like yours, that look for data, and truth.