Pharmacist Driven Shingrix Follow-Up, a Randomized Controlled Trial
Background
Herpes zoster is a vaccine-preventable disease. The CDC and ACIP recently updated guidelines to include Recombinant Zoster Vaccine (RZV or Shingrix) as the preferred vaccine over Zostavax or Zoster Vaccine Live (ZVL). Despite RZV’s increased efficacy, one of its limitations is that it requires two doses compared to ZVL’s single dose. Pharmacy Benefit Managers (PBMs) can leverage the claims data available to them to perform pharmacist/pharmacy intern driven telephonic follow-up to increase adherence to the series and prevent both costly and painful herpes zoster and its secondary effects.
Objective
To determine if pharmacist/pharmacy intern delivered telephonic outreach reminders to a randomized selection of Magellan Rx Medicare Prescription Drug Plan (PDP) participants who had only received one dose of RZV would improve participant adherence with its two-dose vaccine schedule compared to those who did not receive a telephonic outreach reminder.
Methods
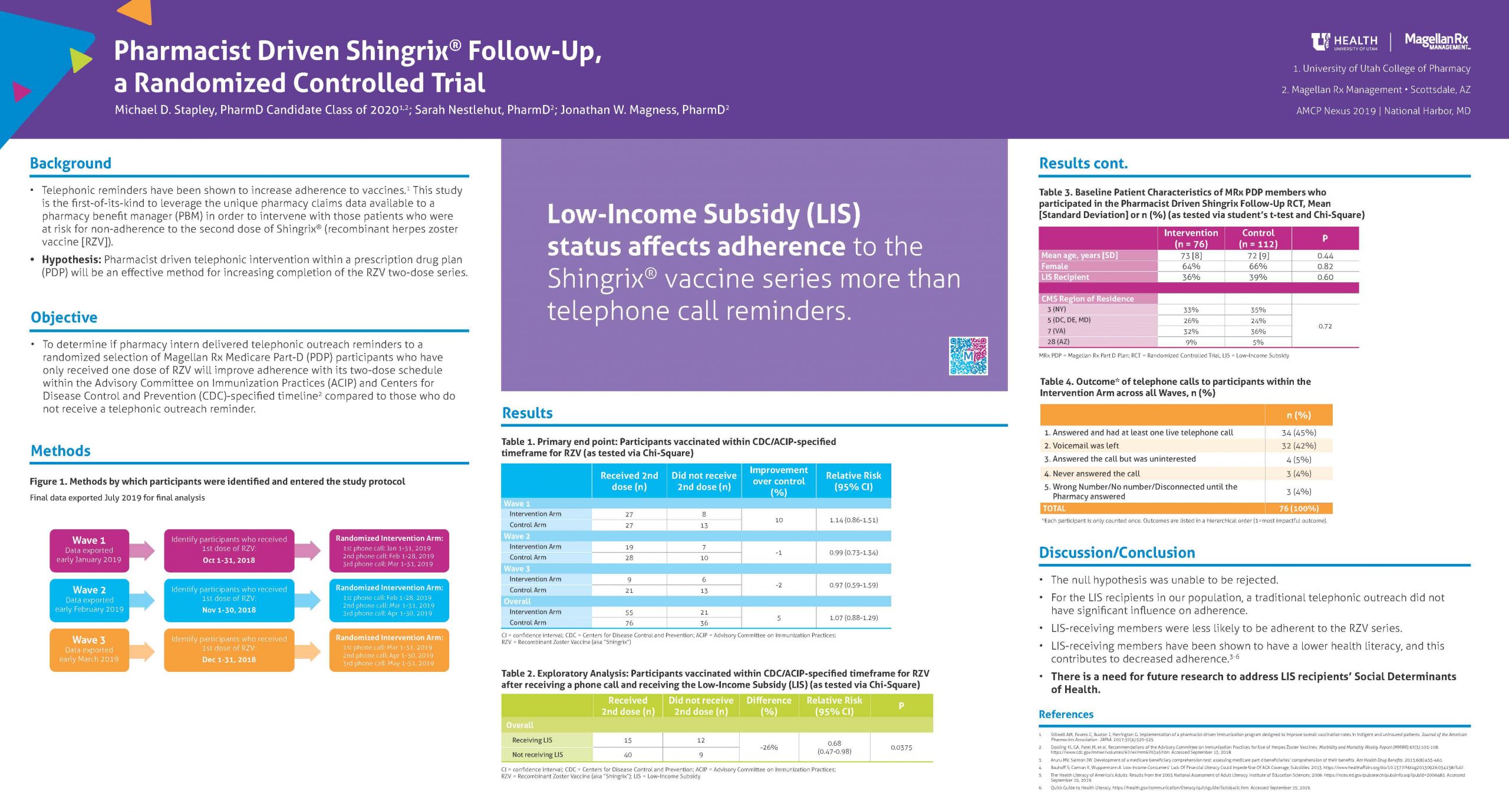
A total of 188 Magellan Rx PDP (MRx PDP) beneficiaries were blinded and randomized into the intervention (n = 76) and control (n = 112) arms. Each beneficiary had only received one dose of RZV at randomization. The study consisted of three “waves,” and phone calls were made to all intervention arm participants when they were 3, 4, and 5 months removed from their initial dose. Final pharmacy claims data were exported in early July 2019, and all participants were reviewed per-protocol to identify whether or not they completed the RZV series.
Results
Compared to control, the intervention group saw a non-significant increase of 4.5% (p = 0.51) in the overall proportion adherent to the complete RZV series. Nine participants in total received their second dose outside of the recommended 6-month time window. In exploratory analyses, receiving a low-income subsidy (LIS) negatively affected adherence to the second dose in both arms of the study, with a composite relative risk of 0.70 (95% CI: 0.55-0.88).
Conclusions
This study lacked sufficient sample size and power for the primary outcome result to be statistically significant. However, in post-hoc analyses, members were significantly less likely to be adherent to the RZV series if they also received a LIS compared to those that did not receive the subsidy. LIS-receiving members have been shown to have a lower health literacy, and this may have contributed to their decreased adherence. There is need for future research to address LIS recipients’ social determinants of health.
Sponsorship
This work was sponsored by Magellan Rx Management, then employer for Stapley, Nestlehut, and Magness.
Published in College of Pharmacy, Virtual Poster Session Spring 2020

Nice work, Michael! What interventions other than phone calls do you think pharmacists could try to help patients complete the vaccine series?
Thank you, Dr. Witt. Thinking specifically of our patients who receive a Low-Income Subsidy, I think the intervention that pharmacists should try is the incorporation of “flags” into the dispensing software (that is hopefully connected to the patient’s greater electronic medical record) that will alert the pharmacist to those patients who are eligible for the vaccine. When the pharmacists are doing their final check of whatever medication the patient is getting, a “Pharmacist Counsel” tag can be included in that patient’s bin. When the patient comes to the pharmacy to pick up their medication, the pharmacist can take the opportunity to discuss the vaccine with them and invite them to get it right then and there.
Do you know what the requirements are to get LIS? It would also be interesting to look at income more directly, since you would hope getting a subsidy does not make the follow up than not getting it with the same income. Of course, that would be much harder information to get.
Thank you for the comment, Dr. Henchey. I agree, it would be interesting to look at income more directly to see if we can parse out any confounders. My understanding is that the low-income subsidy falls under the various “Extra Help” programs available from the U.S. Social Security Administration and/or CMS. The webpage https://secure.ssa.gov/i1020/start describes the requirements. In general, the requirements include: a combined savings, investments, and real estate portfolio not worth more than $29,160, if individual is married and living with their spouse, or $14,610 if the individual is not currently married or not living with their spouse. (Do NOT count the individual’s home, vehicles, personal possessions, life insurance, burial plots, irrevocable burial contracts or back payments from Social Security or SSI.) Furthermore, if the individual has Medicare and Supplemental Security Income (SSI) or Dual Medicare and Medicaid, they will automatically get the extra help.
Hey Michael, I was just curious how the telephone reminder was set up when you called? Did you actually talk to patients or leave messages? Do you think any modification to the telephone reminder could have an impact on patients receiving their second dose?
Hey, Spencer, thanks for the comment. I would call the patients directly and hope to have a live conversation with them. I would call them up to three times (once per month over three consecutive months), if I saw each month that they still hadn’t received the second dose. If they didn’t answer, I would leave a voicemail. I do think that we could explore a modification to the telephone reminder, but I also don’t know how confident I am in live telephone conversations OR voicemails having a really strong positive effect on completion of the 2nd dose (at least in my population with so many low-income subsidy receiving members). Please see my response to Dr. Witt’s question, and let me know if you have other thoughts. Thanks!
Nice study. You mention the study lacked power- but the sample size was fairly large. Did you do a post-hoc power analysis to see how many subjects you would have to study to find a difference? My guess is the number would be very large given the p-value was 0.51. Please comment on whether my notion that the intervention just isn’t effective – and may have been due to the shortage of the vaccine.
Dr. Malone, thanks for the comment! Yes, we did do a post-hoc power analysis to see how many subjects I would need to study to find a statistically significant difference, and we found that a sample size of 1,623 participants per individual study arm would have been required. I definitely don’t disagree with your notion regarding the impact of the shortage of the vaccine. I mention that possible confounder in my limitations section and mention that it’s possible that the shortage especially impacted those members who received the low-income subsidy (LIS). This has not been directly studied, but we would hypothesize this to be the case because the LIS-receiving members are less likely to self-advocate and are more likely to have other social determinants of health (SDOH). Thanks!
Michael – I am intrigued with your outstanding work. From what you responded Dr. Malone, it seems like you did not perform stratified randomization based on LIS. I wonder if you have LIS status at time of randomization. Any other proxy that we can use to help minimize this confounder?
Another question is how you performed randomization? Is this clustered randomization based on pharmacy? Can you describe this more?
Dr. Nui, thank you for your interest. I do believe that we stratified appropriately according to LIS, as seen in “Table 2” and as seen in my final manuscript submitted to your class on Canvas.
We performed randomization based upon birth year. If birth year was odd, the participant would be placed in the intervention arm. If birth year was even, the participant would be placed in the control arm. We learned that is not the best randomization scheme. I hope this answers your question.
Michael-
I saw that you stratify your findings based on LIS. My question was on stratified randomization. As you mentioned that you randomized by birth year (which was not quite good), I don’t think you performed stratified randomization based on LIS. I wonder if you have LIS status at time of randomization. Any other proxy that we can use to help minimize this confounder?
Interesting study Michael. I was curious as to how well the telephonic communication was received by the patients? Were they generally appreciative of the call?
Sean, thanks for the comment! I didn’t administer any sort of qualitative survey to my study participants to scientifically gauge this, but from the tones of voice and words I heard them use/say, I would say that many were very appreciative. I got to have a live conversation with about 45% of the participants that were randomized to the “Intervention Arm.” Some members did not even know there was a second dose at all. So, those were the telephone calls that brought me the greatest satisfaction. Thanks!
Interesting! Very cool that you got to do an RCT. I wonder if some sort of different outreach method would have been better (I know I very rarely answer my phone unless I’m expecting a call). I wonder if text or email would have been better. I know there may be issues with privacy though. Either way – interesting study and well done. 🙂
Taylor, I appreciate your comment! It would have been very interesting to study other communication methods simultaneously. Table 4, the orange table in the poster, shows how many “Intervention Arm” participants I was actually able to have a live conversation with. Seeing that the mean age was 72 years, I wonder how effective those more modern methods (e.g., email, text) would be. In some ways, Ben Ham’s poster looks at the text message side of the adherence equation, and it doesn’t look like that proved to be statistically significantly beneficial. Especially with the Low-Income Subsidy receiving members, I think the in-person pharmacist-patient relationship becomes truly critical. Thanks again.
Michael, very nice poster. Your results are very clearly presented and your conclusions follow logically from the data you’ve presented. I wonder how one might link more tightly the reminder call with the actual receipt of the vaccination. I think the steps the patients need to go through between the call and actually getting the second vaccine is the big hurdle preventing your intervention from having an effect. I wonder if the ability to provide an appointment for getting the second vaccination during the call would change the outcome. I know that would make all the difference in the world for me!
Dr. Keefe, I love your thought! You’re right, there are likely some other more covert confounding factors here. Since I didn’t have a direct relationship with any of the 50+ pharmacies that my 76 intervention-arm participants used for the first dose, I didn’t have access their their schedules to know what appointments I could make. It is not impossible to gain that teamwork, but it would be a challenge for a PBM-initiated intervention. Again, thanks for the great question.
I really like how you organized your poster and made the take-home point is highlighted in the middle. Great job!
Thank you, Robbie!
Hi Michael, great to see your poster after being involved at an early stage. Too bad power was insufficient to reject your null hypotheses, but at least you were able to mine your data for some interesting inferences about LIS recipients in your post-hoc analysis.
Thank you, Dr. Herron! Thanks for your help along the way!