Impact of a Community Based Pharmacy Adherence Monitoring Program
Abstract
To identify the impact that personalized pharmacist interventions have on patient adherence by comparing the proportion of days covered (PDC) between patients who received two interventions to those who received more than two interventions.
Background: Medication adherence rates in patients with chronic diseases range between 40-70% and cause one of the highest preventable costs in the health care system.1 Pharmacists have the knowledge and skills to improve medication adherence.2 Value-based care is one way that pharmacies are incentivized to improve medication adherence through reimbursement from Medicare Part D plans based on pharmacy Star Ratings. PDC is one measurement of adherence and is used to determine Star Ratings adherence metrics. Smith’s Pharmacy can obtain additional reimbursement from insurance companies if their patients’ PDCs meet the targets specified in their contracts with Medicare Part D plans. This project looked at the Adherence Monitoring Program at Smith’s Pharmacy to determine if individualized pharmacist interventions increase adherence determined by PDC.
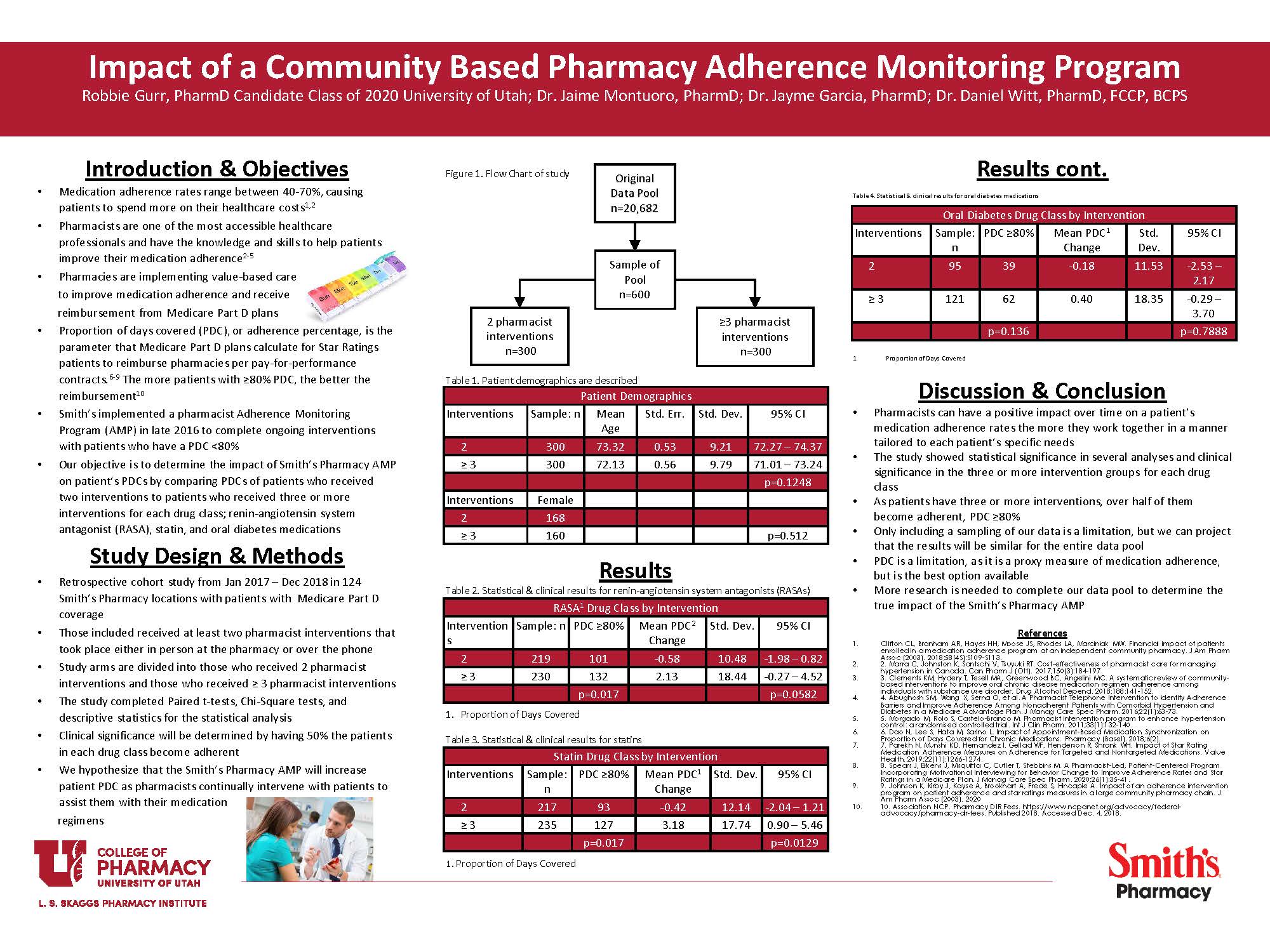
Methods: This study performed a retrospective cohort study to examine the effectiveness of Smith’s Pharmacy Adherence Monitoring Program from January 2017 – December 2018. Those included in this study are patients who had PDCs below 80%, received prescriptions at one of 139 Smith’s Pharmacy locations, had Medicare Part D coverage, and were targeted for and accepted interventions by a community pharmacist. Patients received a personalized intervention through a phone call or in-pharmacy visit to discuss adherence. The study involved reviewing patient data and running several statistical analyses to determine effectiveness, including the Chi-Square test and the Paired t-test through the STATA analysis software program. Interventions were evaluated to determine how the number of adherence encounters between a patient and a pharmacist impacts the patient PDC, comparing patients who received two interventions to those who received three or more interventions. This study aimed to determine the clinical significance of the Adherence Monitoring Program on the patient’s PDC, rather than statistical significance alone.
Results: The mean change in PDCs for each group and medication classes was analyzed using a Paired t-test. The mean change in PDC for patients on a renin-angiotensin system antagonist (RASA) who received two interventions and patients who received three or more was -0.58 PDC% points and 2.13 PDC% points, respectively, with a p-value of 0.0582. The mean change in PDC for patients on a statin who received two interventions and patients who received three or more was -0.42 PDC% points and 3.18 PDC% points, respectively, with a p-value of 0.0129. The mean change in PDC for patients on an oral diabetes medication who received two interventions and patients who received three or more was -0.18 PDC% points and .40 PDC% points, respectively, with a p-value of 0.7888. Those with a PDC above 80% who take RASAs are 233 out of 449 patients, 101 with two interventions and 132 with three or more interventions. The Chi-Square analysis resulted in a p-value of 0.017. Those with a PDC above 80% who take statins are 220 out of 452 patients, 93 with two interventions and 127 with three or more interventions. The Chi-Square analysis resulted in a p-value of 0.017. Those with a PDC above 80% for oral diabetes medication are 101 out of 216 patients, 39 with two interventions and 62 with three or more interventions. The Chi-Square analysis resulted in a p-value of 0.136.
Conclusions: The results of this project show that as patients receive more personalized pharmacist adherence interventions, their adherence, measured by PDC, increases. The study showed clinical significance for the three or more intervention group in each drug class. Smith’s Pharmacy can take these results and find ways to further increase medication adherence within this Adherence Monitoring Program. As pharmacists spend time with their patients through these personalized interventions, they can improve adherence to create better health outcomes, lower healthcare costs, and lead to increased reimbursement from Medicare Part D plans.
Published in College of Pharmacy, Virtual Poster Session Spring 2020
Robbie and Jamie, Great job! I noted that you did not share the interventions on the abstract. Are you able to share the three interventions, at least in some broad fashion, with me?
Thanks
Dr. Munger, thank you! All of the interventions in the Adherence Monitoring Program are personalized to each patient individually. The pharmacists focus on what patient-specific barrier is causing the non-adherence. For example, if a patient is not taking their medication because it is not being administered correctly and causing an upset stomach, the pharmacist would counsel on proper administration. The same would go for any barriers, including cost, side-effects, and any others. In conclusion, the pharmacist uses all of their resources and knowledge to do all that they can to help the patient overcome these barriers of non-adherence.
This is an excellent project to show the importance of pharmacists. It is valuable to see the effects based on the significance of your findings.
Thank you. Yes, it is great to see the impact that pharmacists can make.
This was a valuable research finding. Thank you.
You’re welcome. Thank you.
Robbie, Nicely presented poster, with the results clearly presented and described! Can you remind me why you used at least 50% of the patients adherent (based on PDC of ≥80%) as your measure of a positive clinical outcome of the intervention? In your introduction you note that adherence rate range between 40-70%. It seems to me that 50% falls right in there, so achieving 50% adherence rate would not address the problem. Am I thinking about this incorrectly?
Dr. Keefe, so the project was defining clinical significance as having half, or 50%, of the patients enrolled in each study arm to become adherent, which is having a PDC greater than or equal to 80%. For example, if we were to get 150 out of 300 patients at a PDC of 80% or higher, we can conclude that clinical significance was met. This shows that the study was able to get 150 or half the patients adherent when they weren’t adherent at the beginning of the study. I hope that this makes sense. If it does not, I would be more than willing to explain over a phone call when you have time.
Robbie – interesting piece of work. This is not a question. It’s more like a comment. I am concerned that patients that received 2 interventions must be different from those receiving >3 pharmacists interventions. I can see the better adherence among those receiving >3 pharmacists interventions. However, i wonder if there is any differences between 2 groups other than pharmacist interventions that might be the reasons for better adherence. I would feel that stating “pharmacy can have a positive impact on patient adherence” is a bit too strong to say. Just my two cents.
Thank you for your comment. I do agree that there are some limitations that are within the study and not knowing much about the patient demographics is not helpful.
Nice job, Robbie. You did a nice job pulling everything together. What is one thing you learned while doing this project that you think you’ll apply in your future career?
Dr. Witt, thank you. One thing that I believe will help me in my career going forward is to ensure that there is an understanding at the beginning of a project and that there are clear communication and feedback given throughout the process to get the best results possible. This can also refer to a new clinical program or something similar that is implemented at a pharmacy. Having an accurate understanding of what the goal is, is vital to success. I believe that I have learned things through this project that will make me a better pharmacist.
Great job, Robbie! When you compared the 2 intervention arm to the ≥3 intervention arm, it looked like the P-value was not <0.05 in the oral diabetes drug class. Any idea why there were statistically significant differences in the RASAs and Statins groups but not in the diabetes drug class?
Thank you, Michael. Where there were not as many patients taking an oral diabetes medication, I don’t think we had enough patients to show a statistically significant difference. Along with that, the mean change in PDC was closer together in the diabetes class than the RASA and statin groups, so there wasn’t much of a difference in that regard. I hope that makes sense to you.
Yes, that does make sense, thanks. So, it was just a sample size/power issue or do you think there are other conclusions that can be made about some other inherent difference in the oral diabetes medication class?
Nice study. I was surprised that the mean change in PDC was so small, yet statistically significant. Can you comment on the clinical significance of this finding (increase of PDC by slightly more than 2%)?
The clinical significance of this project was by having half the patients in each medication class become adherent, which is a PDC of 80% or greater. This is the parameter that is set by Medicaid of having patients adherent, anything less than 80% is considered non-adherent. By having half of the patients reach this parameter in the study, it made it so that Smith’s had better Star Ratings from Medicaid, which allows for greater reimbursement. Many of the patients were within the 70-79%, which allowed for such a small change in PDC to be so significant. If you have more questions or if it doesn’t make total sense, let me know.
Nice work Robbie! This was a cool study.
Thanks Sean!
Bravo Robbie! I enjoy seeing projects where pharmacists make it a point to involve the patient in dynamic aspects of care! In this case, making the patient an important part of the pharmacy health care team! Now to look at this program and long term consequences. Excellent poster! Thank you!!
Thank you, Dr. Orlando. Yes, it will be fascinating to see what the data will look like in the long run and as time goes on. We would hope that it would continue to help patients become more adherent to their medication regimens.
Robbie, nice job. Is this something you could also present at UPhA?