Evaluation of the Neurocritical Care Insulin Infusion Protocol within the University of Utah Neurocritical Care Unit
ABSTRACT
Background
There are no generally recognized guidelines regarding insulin therapy in neurologically injured patients. Utilizing a protocol that results in high rates of hyperglycemia or hypoglycemia can be extremely harmful in this patient population. The University of Utah updated their insulin infusion protocol in December 2015. Since that time, no quality assurance studies have been done to ensure the chosen glucose range of 121-180mg/dL is safe for this population.
Methods
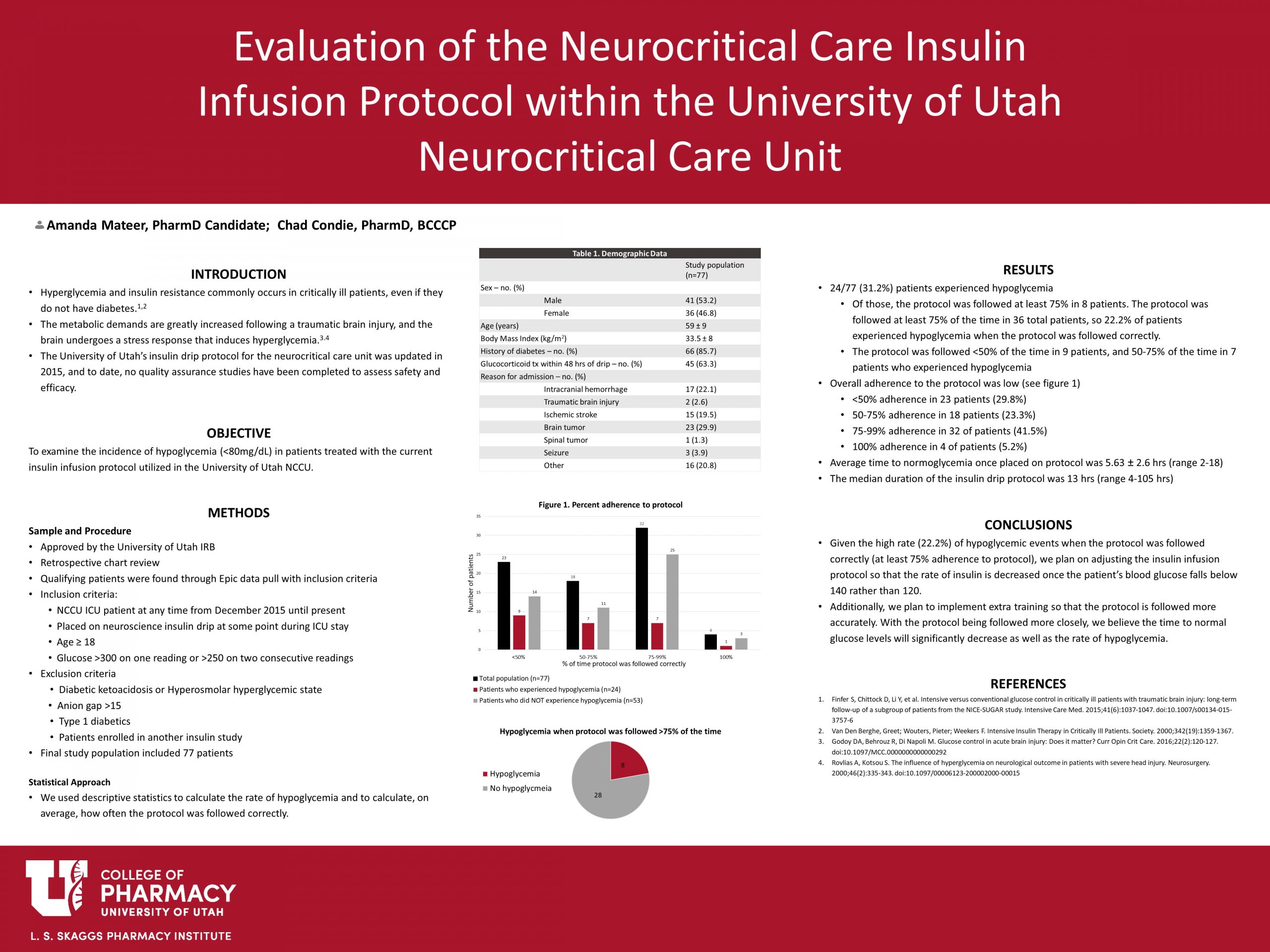
We will be performing a retrospective chart review to determine the rate of hypoglycemia (blood glucose <80mg/dL) among all patients placed on an insulin drip from December 2015 until July 2019. The electronic medical record (EMR) will be used to identify patients who meet the inclusion criteria. We will calculate the frequency of hypoglycemia (glucose <80mg/dL) among our population. We will also evaluate the level of compliance in following the protocol (100% of the time, 75-99% of the time, 50-74% of the time, or <50% of the time). If the rate of hypoglycemia is >5%, we plan to revise the protocol.
Results
Data was available for 77 patients. 24 patients (31.2%) experienced hypoglycemia (BG <80). The protocol was followed at least 75% of the time in 8 of the 24 hypoglycemic patients. The protocol was followed <50% of the time in 9 of those patients, and 50-75% of the time in 7 patients. Overall adherence to the protocol was low with the protocol being followed <50% in 29.4% of patients. The average time to normoglycemia once placed on the protocol was 5.63 hours, with a range of 2 to 18 hours. The median duration of the insulin drip protocol was 13 hours, with a range of 4 to 105 hours.
Conclusions
Given the high rate of hypoglycemic events when the protocol was followed correctly, we plan on adjusting the insulin infusion protocol so that the rate of insulin is decreased once the patient falls below a blood glucose of 140 rather than 120. Additionally, we plan to implement extra training so that the protocol is followed more accurately.
Published in College of Pharmacy, Virtual Poster Session Spring 2020
Wow – this is an impressive project! It is so cool that your findings were actually used to change practice. Did you get to have any input on what the extra training would look like moving forward? Amazing work, Amanda!
Thanks Chelsea! I believe Chad (pharmacist in the NCCU) planned an in-service to review the protocol with the NCCU staff.
It’s exciting that your project is already leading to improvements in the protocol!
Yes – it’s great to see some results from all this hard work! 🙂
Great work Amanda. As has already been said, it’s wonderful to see that your research/inquiry is going to make a difference in clinical practice! How does that feel? Do you have a sense as to why the protocol is not followed? Also, when it is not followed, does that mean a patient is more likely to remain hyperglycemic, or can it be that too much insulin is given and patients develop hypoglycemia as well?
Hi Dr. Keefe,
It feels great to have made a difference in clinical practice. It’s hard to say why the protocol wasn’t being followed. I’m thinking it is a lack of accurate charting and/or the nurses just weren’t sure what the protocol was. With our results, it seemed like there was a higher chance of hypoglycemia when the protocol was not followed. However, we saw a bit of both hyperglycemia and hypoglycemia.
Great job!
Thanks, Robbie!