Effects of Bowel Protocol Adherence on the Need for Emergency Bowel Medications in a Neuro Critical Care Population
Introduction: Constipation and its associated comorbidities are major concerns for hospitalized neurocritical care patients. Many institutions implement scheduled maintenance bowel regimens as an attempt to prevent constipation in these patients. In this study, we examined if strict adherence to a daily bowel regimen can prevent the need for rescue therapies.
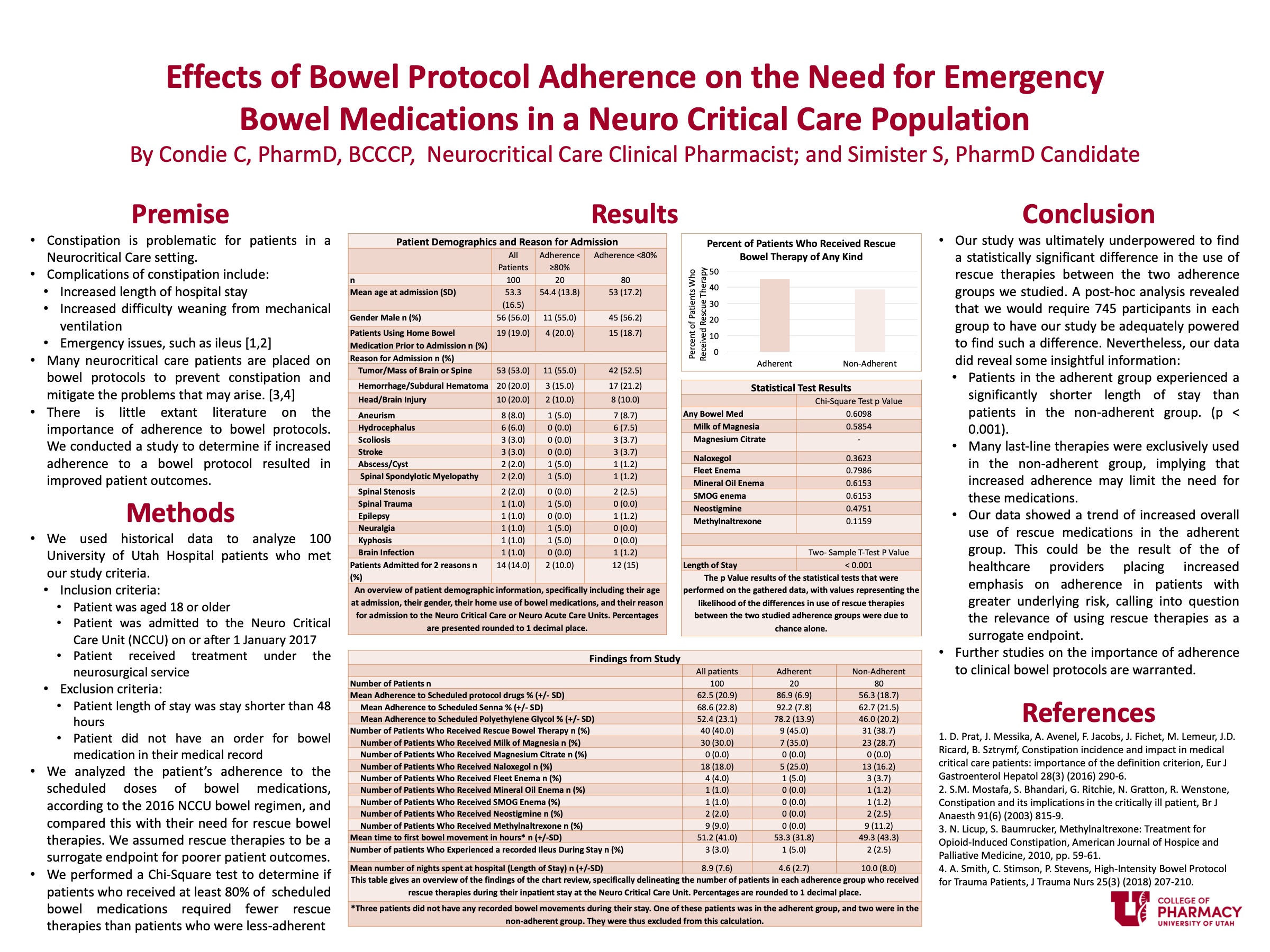
Methods: We conducted a retrospective review on 200 Neurocritical Care patients at the University Of Utah Hospital. These patients were assessed for adherence to the scheduled maintenance bowel medications, as well as the frequency at which they required the use of the rescue bowel medications. We then looked to determine if there was a statistical difference in the use of rescue medications in patients who received 80% or more of the scheduled bowel regimen medications (adherent group) versus those who received less than 80% of the scheduled bowel regimen medications (non-adherent group).
Results: 20% of the patients we studied received 80% or more of the scheduled bowel medications. 45% of patients in adherent group required a rescue therapy, compared to 38.7% of patients in the non-adherent group. The P value obtained from the chi-squared test performed on these values was 0.6098.
Conclusion: Our study failed to show a statistically or clinically significant difference between the two adherence groups that we analyzed. This study does, however, lay the foundation upon which future studies could further analyze the importance of bowel protocol adherence.
Published in College of Pharmacy, Virtual Poster Session Spring 2020
Spencer, nicely presented poster! I am still fascinated by the prospect that in patients in an NCCU can be non-adherent. Does this really mean that the providers (e.g., doctors, nurses) are not adherent with the orders? Or are the patients truly non-adherent (e.g., refusing treatment)? If the former is the case, then why do you think that the majority of patients are not being given the bowel therapies as ordered? Your data might suggest that adherence to these doesn’t really seem to matter; perhaps providers have realized that and so aren’t so concerned about adhering to the protocol?
Hello, Doctor Keene,
Thank you for your response. That is a great question. While I was collecting the data for this study, I noticed that there were several reasons noted for why patients did not receive scheduled doses of their bowel medications. Sometimes, it was noted that the patient or family refused the medication. Sometimes, the providers elected to hold the dose due to the patient having recently experienced a regular bowel movement, and sometimes it was held because the patient had experienced diarrhea/loose stools. While I did not specifically record or analyze these reasons for the purpose of my study, I feel that future research on the topic could definitely look into these reasons for non adherence, and possibly see how patient outcomes differ in relation to the reason their therapy was held – That may be able to shed light on whether or not the provider’s decision to hold therapy is truly beneficial to the patient.
Sorry. Autocorrect butchered your name, Doctor Keefe.
Nice work on your analysis and poster. I was wondering what may have contributed to poor adherence? I was also wondering what you used to define as being adherent vs non adherent. Was it based on missing a single dose? or was it based on missing an X number of doses? I think it would be interesting to move it into quartiles then compare outcomes at 25%, 50%, 75%, and 100% adherence. It would give the clinician a real work view of use of rescue medications. Did you by chance assess or look at medications that can reduce motility such as opioids and compare that to the use rescue medications? Thank you
Hello, Kimmy,
Thank you for your comment. Those are all very good questions! In several cases where patients did not receive the scheduled medications, the doses were either refused by the patient or family, or it was withheld due to the patient having either recently experienced a bowel movement or were actively experiencing diarrhea. For my study, however, I did not, specifically go into these individual reasons for the analysis I performed, though it would definitely be an excellent area that future studies could delve into further. Adherence was assessed by determining the total expected scheduled doses that a patient should have received during their stay, according to the 2016 NCCU bowel protocol, and comparing it to how many doses of those medications the patient actually received. ((Doses administered/doses expected)*100%) My study did not specifically make assessments of the medications that can reduce motility, such as opioids, though it is true that they can have an impact on constipation. Opioids, among other factors such as surgeries and decreased mobility, all contribute to increased concern for constipation in NCCU patients, and further research in this field going forward could help further shed light on determining ways that patient outcomes can be improved, so that optimal therapy can be provided. If you have not yet seen Sean Christensen’s poster, I definitely recommend giving it a glance. His project also looked at NCCU patients, but his focus was on seeing differences in patient outcomes between the previous and the current NCCU bowel regimens, and it shows how alterations in bowel regimen medications affect patient outcomes.
Hi Spencer! This is a very important subject for management of these specialized patients. Of only 20% of pts received 80% of the bowel protocol, what were the barriers that prevented a higher utilization rate? As a pharmacist, what role could you play to compliment these utilization rates in a multi-disciplinary team setting as the NCC. Nice work! Thank you for sharing this important data!
Hello, Doctor Orlando,
Thank you for your comment and questions! It definitely is an important subject, and increasing adherence to medication use (both on the end of patients self-medicating as well as healthcare providers administering medications to inpatients) seems to be an ongoing ‘labor of love’ for many pharmacists – I even remember when I was on rotation with you a few months ago that we were involved with monitoring the OPAT patients, and we had a few concerns about patients who did not adhere to their dosing, or who did not change the dose they were administering as we recommended them to do. For the patients I evaluated for this study, it was noted in several cases that the medication was refused by the patient or their family. As such, pharmacists can help play an important role by ensuring that patients receive adequate and appropriate counseling on the utility and purpose of the medications ordered for them, so as to avoid decreased adherence from patient refusal. Another thing that pharmacists can do on an interdisciplinary team to help improve patient outcomes is to assist in developing, updating, and maintaining the medication protocols so that they are up-to-date with current literature and recommendations. The NCC bowel protocol was actually updated in 2016 to place a greater emphasis on the use of PEG instead of Docusate (given its improved relative efficacy) and one of my classmates conducted their project to analyze the difference that this change had on patient outcomes.
Spencer, sometimes, the best, and most important, scientific analysis determines there is no difference. nice job.
Hello, Doctor Ruble,
Thank you so much for your comment. I couldn’t agree more. The purpose of science is to advance the collective knowledge and understanding of mankind, and determining no difference in a study advances that knowledge just as much as determining a difference. Unfortunately, of the two, the latter typically makes it to publication much more frequently.